Neuro-Ophthalmology
Understanding Neuro-Ophthalmology
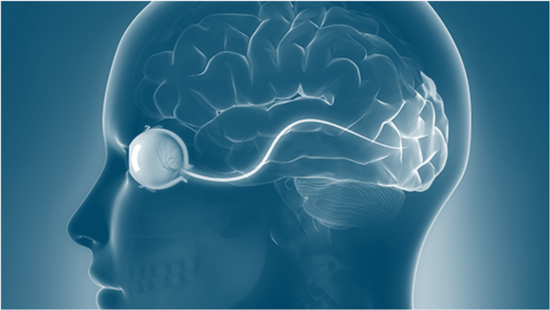
Neuro-Ophthalmology is a subspecialty that merges the fields of neurology and ophthalmology, often dealing with complex systemic diseases that have manifestations in the visual system. The neuro-ophthalmologists at Nandadeep are adept at diagnosing and treating conditions that affect the optic nerve, the visual pathways, and the eye movement systems.
Comprehensive Eye Care Treatments Under One Roof
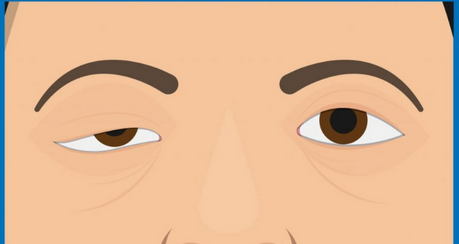
Diplopia (Double Vision)
Diplopia, or double vision, is a condition where an individual sees two images of a single object. This visual impairment can be either monocular or binocular:
- Monocular Diplopia: This occurs when double vision is present in only one eye. The second image is often a fainter “ghost” image and can be caused by issues within the eye itself, such as cataracts or refractive errors.
- Binocular Diplopia: This type occurs when both eyes are open and is often due to the eyes not aligning properly. The double vision disappears when one eye is covered. Causes can include strabismus, nerve damage, or muscle disorders.
Symptoms
Symptoms of diplopia can include overlapping images, misaligned views, and difficulty with depth perception.
Treatment
Treatment for diplopia aims to address the underlying cause and may involve corrective lenses, eye patches, surgery, or prism glasses to help align the images.
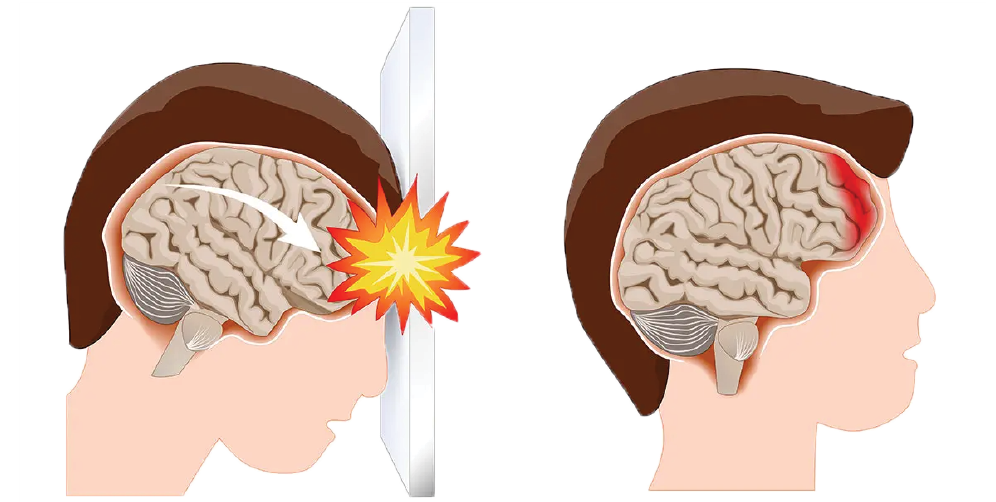
Traumatic Brain Injury (TBI)
A TBI is caused by a sudden trauma to the head, leading to damage to the brain. TBIs can range from mild concussions to severe brain injuries and can have various causes, including falls, vehicle accidents, sports injuries, or violence.
Symptoms
Symptoms of TBI can be physical, cognitive, or sensory, and may include:
- Physical Symptoms: Headaches, nausea, vomiting, dizziness, blurred vision, sleep disturbances, and seizures.
- Cognitive Symptoms: Confusion, memory loss, attention deficits, and mood swings.
- Sensory Symptoms: Sensitivity to light or sound, vision problems, and balance issues.
Treatment
The treatment for TBI is multifaceted and depends on the severity of the injury. It can include emergency care, surgery, medications, and vision rehabilitation therapies and vision therapy. The goal is to stabilize the patient and work on recovering as much function as possible.
Papilledema
Papilledema is the swelling of the optic disc, the point where the optic nerve enters the retina, due to increased intracranial pressure (ICP). It’s almost always bilateral, affecting both eyes.
Symptoms
- Visual Changes: Brief episodes of blurred vision, double vision, flickering, or complete loss of vision, typically lasting seconds.
- Headaches: Often worse in the mornings or when lying down.
- Nausea and Vomiting: Due to the elevated ICP.
- Neurological Symptoms: Such as problems with movement or thinking, depending on the underlying cause.
Causes
Papilledema can be caused by a variety of conditions that lead to increased ICP, including:
- Brain tumours
- CNS inflammation
- Cerebral venous thrombosis
- Idiopathic intracranial hypertension (IIH)
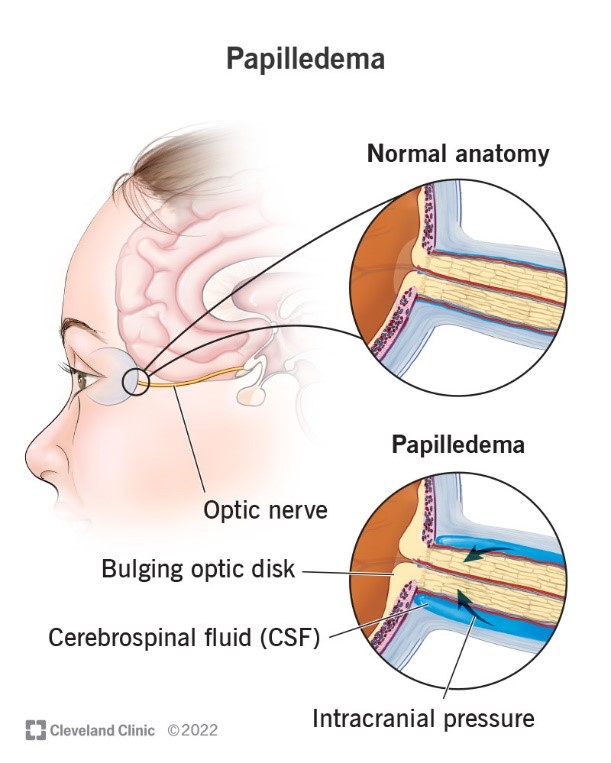
Treatment
The treatment of papilledema involves addressing the underlying cause of increased ICP. This may include medication to reduce ICP, surgery to relieve pressure, or other treatments specific to the underlying condition.
External Ophthalmoplegia
External ophthalmoplegia refers to the weakness or paralysis of the eye muscles, affecting the ability to move the eyes. It can be chronic and progressive, known as chronic progressive external ophthalmoplegia (CPEO), or it can occur suddenly because of an acute condition.
Symptoms
- Ptosis: Drooping of the eyelids, which can affect one or both eyelids.
- Ophthalmoplegia: Weakness or paralysis of the muscles that move the eye, leading to difficulty controlling eye movements.
- Diplopia: Double vision due to the misalignment of the eyes.

Causes
It is often associated with mitochondrial diseases and can occur as isolated oculomotor symptoms or in conjunction with other systemic findings. It can also be caused by muscle disorders or other conditions that disrupt the messages sent from the brain to the eyes.
Treatment
Treatment for external ophthalmoplegia focuses on managing symptoms and may include eyelid surgery for ptosis or strabismus surgery to correct eye alignment. In cases associated with mitochondrial disease, supportive treatments and genetic counselling may be offered.
Cerebral Palsy and Vision
Cerebral palsy (CP) is a group of disorders that affect movement, muscle tone, and posture. It is caused by damage to the developing brain, often before birth. Vision problems are common in children with CP due to the brain damage that causes the disorder. In fact, studies have shown that up to 75% of children with CP experience some form of vision impairment.
Types of Vision Impairments in CP:
- Cortical Visual Impairment (CVI): This is the most common type of visual disability in CP, caused by brain damage rather than an issue with the eyes themselves. Symptoms can include difficulty focusing, blurred vision, field vision loss, and problems recognizing familiar faces.
- Strabismus: This condition involves the eyes turning in different directions and can lead to blurred vision and amblyopia, also known as "lazy eye".
- Hyperopia (Farsightedness): This is another visual impairment that can affect children with CP, where distant objects may be seen more clearly than those that are near.
Treatment
Treatment for vision problems in CP includes regular screenings, prescription glasses, contact lenses, or other visual aids. In some cases, surgery may be necessary to control eye movement.
Concussion and Vision
A concussion is a type of traumatic brain injury (TBI) caused by a blow to the head or body that results in rapid movement of the brain inside the skull. This can lead to a variety of symptoms, including those that affect vision.
Vision-Related Symptoms of Concussion
- Double Vision: Difficulty with the eyes working together, which can result in seeing double.
- Sensitivity to Light: Increased discomfort from bright lights or glare.
- Eye Tracking Problems: Difficulty following moving objects or shifting focus between targets.
- Visual Fatigue: Eyes tiring easily, leading to headaches and difficulty concentrating.
Treatment
Concussions can cause these vision problems by disrupting the neural pathways associated with the visual system. Treatment may involve rest and gradual return to activities, but some cases require more specialized care, such as vision therapy or corrective lenses.

Optic Atrophy
Optic atrophy refers to the damage and subsequent degeneration of the optic nerve fibers, which can lead to vision loss. This condition can be caused by various factors, including:
- Lack of proper blood flow (vascular/ischemia): This is the most common cause of optic nerve atrophy.
- Inherited conditions: Such as Leber hereditary optic neuropathy, which causes vision loss first in one eye, then the other.
- Pressure: Either from tumors or conditions like glaucoma that can damage the optic nerve.
- Inflammation: Diseases or swelling in the optic nerve itself, such as optic neuritis.
- Infections: Diseases like syphilis and measles can lead to optic atrophy.
- Trauma: Eye injuries from accidents or sports can cause optic atrophy.
- Retinal diseases: Conditions like diabetes-related retinopathy and retinal vein occlusion can affect the optic nerve.
- Toxins, nutritional deficits, or medications: These can usually affect both eyes.
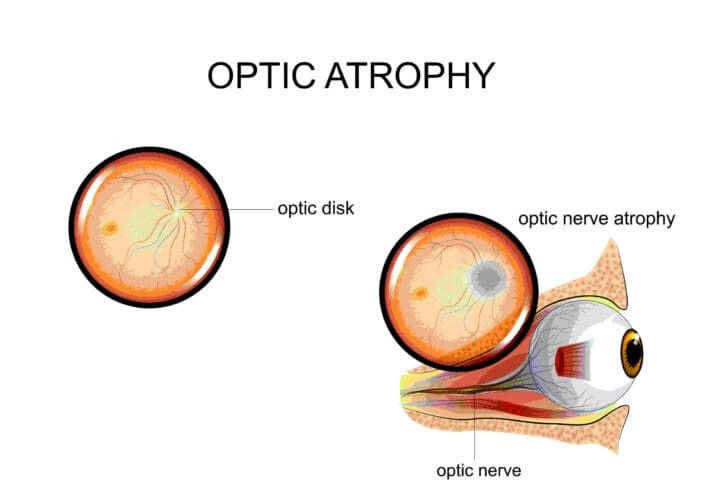
Symptoms
Symptoms of optic atrophy can include blurred vision, difficulties with peripheral vision, and difficulties with color vision. While optic atrophy itself is not reversible, treating the underlying causes can help to stop the progression of the disease.
Optic Neuritis
Optic atrophy refers to the damage and subsequent degeneration of the optic nerve fibers, which can lead to vision loss. This condition can be caused by various factors, including:
- Eye pain: Especially with eye movements.
- Vision loss in one eye: Can range from mild to severe.
- Visual field loss: Loss of side vision in various patterns.
- Loss of colour vision: Colours may appear less vivid than normal.
- Flashing lights: Some people report seeing flashing lights with eye movements.
The exact cause of optic neuritis is not fully understood, but it is believed to develop when the immune system mistakenly attacks the myelin covering the optic nerve, leading to inflammation and damage. Conditions that can cause optic neuritis include multiple sclerosis, neuromyelitis optica, and infections such as Lyme disease, as well as diseases like lupus and sarcoidosis.
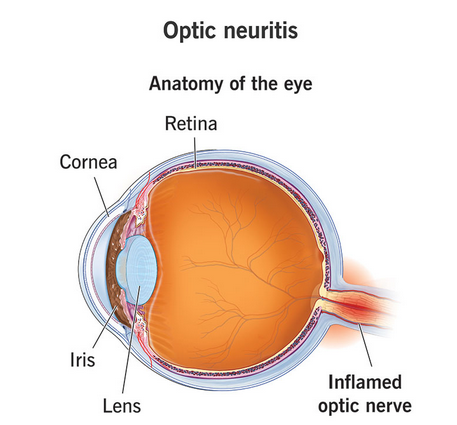
Diagnosis of optic neuritis involves a comprehensive eye examination and imaging tests like MRI to study the brain and orbits. Treatment often includes steroids to reduce inflammation in the optic nerve. In some cases, plasma exchange therapy or intravenous immune globulin (IVIG) therapy may be used, especially when steroid therapies are not effective.
Myasthenia gravis (MG)
It is an autoimmune disorder that primarily affects the neuromuscular junction—the connection between nerves and muscles—leading to muscle weakness and fatigue. It is particularly significant because it often presents with symptoms related to eye movements and eyelid function.
Symptoms
- Ptosis: Drooping of one or both eyelids.
- Diplopia: Double vision due to weakness of the muscles that control eye movements.
- Variable extra-ocular muscle palsies: Inconsistent weakness in the muscles that move the eyes, which can lead to misalignment and double vision.
- External ophthalmoplegia: Paralysis of the eye muscles.
Diagnosis
Neuro-ophthalmologists may use various tests to diagnose MG, including:
- Edrophonium test: Administration of a drug that temporarily increases the levels of neurotransmitters at the neuromuscular junction, which can improve muscle strength in MG patients.
- Repetitive Nerve Stimulation (RNS): A test to detect abnormal muscle response to nerve stimulation.
- Single Fiber EMG: Measures the electrical activity of individual muscle fibers.
- Ice test: Application of ice to the eyelids, which can temporarily improve ptosis in MG patients.
Treatment
- Medical therapy: Includes medications like anticholinesterase agents that improve neuromuscular transmission and immunosuppressive drugs to reduce antibody production.
- Surgery: Thymectomy, the removal of the thymus gland, may be considered in some cases.
- Monitoring: Regular follow-up is crucial as ocular MG can progress to generalized MG, affecting other muscles in the body.
Schedule a Consultation
Talk to our neuro-ophthalmologist at Nandadeepe Eye Hospital to discuss your concerns and get personalized treatment recommendations.
Our Neuro-Ophthalmology Experts
Dr. Sourabh D. Patwardhan
Phaco-Refractive-Vitreoretina- Glaucoma specialist FRCS (UK), MS (AIIMS), DNB, MNAMS, FICO


