What is Keratoconus? Symptoms, Diagnosis, and Treatments
Introduction
Have you ever realized that your eyesight is becoming blurrier with time, even after obtaining new glasses? Or have you become more sensitive to bright lights?
These are the symptoms of keratoconus, a progressive eye condition that affects the cornea, the clear front surface of the eye. Understanding keratoconus is very important because early detection and appropriate treatment can preserve vision and improve quality of life.
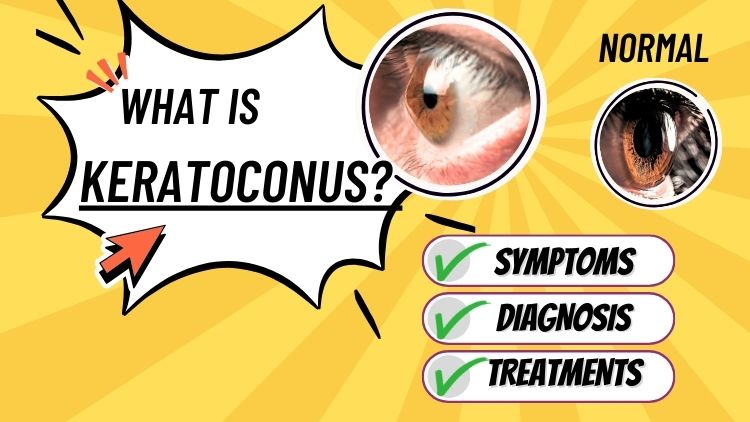
What is Keratoconus?
Keratoconus is a condition in which the cornea, typically spherical and dome-shaped, becomes thin and starts growing outward into a cone shape. This shape alteration affects how light enters the eye, resulting in blurred or distorted vision.
Keratoconus commonly develops in youth or early teenage years and can last up to the 30s. Keratoconus, if left untreated, can cause considerable vision loss and interfere with daily activities such as reading, driving, and watching television.
Symptoms of Keratoconus
Early signs of keratoconus might be minor and may include:
- Blurred or distorted eyesight (straight lines can appear wavy or twisted)
- Enhanced sensitivity to light and glare
- Frequent modifications in eyeglass prescriptions do not appear to improve much.
As the condition develops, you might notice:
- Increasing nearsightedness (myopia) and astigmatism (irregular curve of the eye).
- Difficulty seeing clearly with glasses or soft contacts
In extreme cases, corneal scarring or sudden vision loss may occur due to corneal hydrops, a condition caused by sudden swelling of the cornea.
It’s crucial to note that keratoconus frequently affects both eyes, though not usually equally.
Diagnosis of Keratoconus
If you’re experiencing symptoms, an eye doctor can do several tests to diagnose keratoconus:
- Eye Refraction: Measures how well you see at different distances and aids in the determination of your prescription.
- Slit-Lamp Examination: A special microscope is used to detect evidence of corneal thinning or scarring.
- Keratometry assesses the curvature of your cornea.
- Corneal Topography or Tomography: This technique creates a precise map of your cornea’s shape and thickness, making it the most effective way to diagnose keratoconus even in its early stages.
- Pachymetry is the measurement of your cornea’s thickness.
Early detection is especially crucial if you are considering laser eye surgery, as keratoconus may make you ineligible for some operations.
Treatment Options for Keratoconus
Treatment is determined by the severity of the illness.
Corrective Lenses: First Step
For many people with mild to moderate keratoconus, glasses are their first line of defense. They can give excellent vision correction when the corneal changes are minimal.
As the illness advances, glasses may no longer provide clear vision. This is when specialized contact lenses come into action.
- Soft contact lenses: It help in the initial stages of keratoconus, but as the condition progresses, they fail to restore the vision.
- Scleral contact lenses: These lenses are placed over the cornea and white area of the eye, offering comfort and stability even when the cornea isn’t in its proper shape.
Corneal Cross-Linking (CXL): Stopping Progression
Corneal cross-linking is an effective treatment for increasing the strength of the cornea and slowing the rate of progression of keratoconus. During CXL, your doctor inserts riboflavin (vitamin B2) eye drops into the cornea, projecting certain ultraviolet (UV) light into the eye. This process forms new links between the cornea’s collagen fibers, making it tougher and less prone to expand further.
CXL can not reverse keratoconus, but it can keep it from worsening, especially if detected early. It is the only FDA-approved medication for slowing or stopping the progression of the disease.
At Nandadeep Eye Hospital, our keratoconus eye specialists offer advanced corneal cross-linking techniques to prevent the condition from worsening and help patients maintain stable and functional vision.
Intacs (Corneal Implants): Reshape the Cornea
For people who cannot attain satisfactory vision with lenses alone, Intacs may be advised. Intacs are small, arc-shaped implants that are surgically inserted into the cornea. Their job is to flatten and shape the cornea, which can improve vision and make contact lenses more comfortable to use.
The method is quite short and can be paired with cross-linking for the best outcomes. Intacs can not prevent keratoconus from advancing, but they can postpone the need for a corneal transplant in many situations.
Keratoplasty (Corneal Transplant): for advanced cases
When keratoconus gets severe, such as when the cornea is exceedingly thin, scarred, or when eyesight cannot be corrected with existing therapies, a corneal transplant may be required. This procedure involves replacing a portion or all of the corneal transplant with healthy donor tissue.
There are two primary types:
- Penetrating Keratoplasty (PKP) is a full-thickness transplant that replaces the entire cornea.
- Deep Anterior Lamellar Keratoplasty (DALK) involves replacing only the cornea’s front layers, leaving the healthy inner layer intact.
Corneal transplants are generally effective, however, they are reserved for patients if other therapies have been unsuccessful.
Eligibility Criteria
Ideal candidates for refractive surgery:
- Are 18 years or older
- Have had a stable eyeglass prescription for at least one year
- Have healthy corneas and no major eye conditions.
People with keratoconus, severe dry eyes, autoimmune disorders, or uncontrolled diabetes may not be eligible. Pre-operative assessments, including corneal topography and eye health evaluations, are vital to determine suitability.
Living with Keratoconus
Keratoconus treatment is a lifetime procedure. Here are a few tips:
- Regular Eye Exams: Schedule check-ups to monitor changes and adjust treatment as required.
- Avoid Eye Rubbing: Rubbing your eyes can worsen keratoconus.
- Manage Allergies: It will help minimise the need to rub your eyes.
Conclusion
Keratoconus can be a difficult condition, but with early discovery and appropriate treatment, most people can maintain good vision and enjoy busy lifestyles. If you detect changes in your eyesight or have a family history of keratoconus, schedule an appointment with top eye experts near you. People dealing with this ailment now have greater hope than ever because of advances in treatment.
Take care of your eyes- your vision is worth it!
More Posts
Everything You Should Know About Pediatric Eye Exams

काचबिंदू (Glaucoma): नियमित नेत्रतपासणी का आवश्यक आहे?